LMNOP Heart Failure: A Must-Read Guide for Well-Being
Heart disease is a leading cause of death, yet preventative steps and new therapies – like polypills – offer hope. Understanding arrhythmias, cardiomyopathy,
and the impact of heart attacks and arteriosclerosis is crucial for well-being.
Understanding Heart Failure
Heart failure doesn’t mean the heart stops beating; it signifies an inability to pump blood effectively to meet the body’s needs. This often leads to blood backing up, causing fluid accumulation in the lungs and extremities. Several underlying conditions can contribute to this, making a comprehensive understanding vital for proactive management.
A key factor is cardiomyopathy, a disease of the heart muscle itself, hindering its pumping ability. Irregular heartbeats, known as arrhythmias, disrupt the coordinated electrical signals essential for efficient contraction. These disruptions can exacerbate heart failure or even trigger it. Furthermore, a prior heart attack, resulting from blocked arteries, can permanently damage the heart muscle, diminishing its functional capacity.
Arteriosclerosis, the thickening and stiffening of arteries, also plays a significant role by restricting blood flow to the heart, increasing its workload and potentially leading to failure. Recognizing these interconnected factors is paramount for effective prevention and treatment strategies, ultimately improving quality of life.
What is Heart Failure?
Heart failure occurs when the heart muscle is unable to pump blood as efficiently as it should to meet the body’s demands. It’s not a sudden event, but often a gradual decline in heart function. This doesn’t mean the heart stops working entirely; it simply struggles to keep pace with the body’s needs, leading to a cascade of physiological consequences.
The reduced pumping action causes blood to back up in the veins and arteries, resulting in fluid buildup in the lungs, abdomen, legs, and feet. This congestion contributes to symptoms like shortness of breath, fatigue, and swelling. Importantly, heart failure is a complex syndrome with various underlying causes, not a single disease.
These causes range from coronary artery disease and high blood pressure to valve problems and cardiomyopathy. Understanding the specific type of heart failure – whether it affects the left side, right side, or both – is crucial for tailoring appropriate treatment strategies and improving patient outcomes. Early diagnosis and intervention are key to managing this condition effectively.
The Role of the Heart Muscle (Cardiomyopathy)
Cardiomyopathy represents a disease of the heart muscle itself, directly impacting its ability to effectively pump blood throughout the body. This condition makes the heart work harder, potentially leading to heart failure. There are different types of cardiomyopathy, each affecting the heart muscle in unique ways – dilated, hypertrophic, and restrictive being the most common.
Dilated cardiomyopathy causes the heart chambers to enlarge and weaken, reducing pumping efficiency. Hypertrophic cardiomyopathy involves thickening of the heart muscle, making it harder for the heart to relax and fill with blood. Restrictive cardiomyopathy stiffens the heart muscle, limiting its ability to stretch and fill properly.
Regardless of the type, cardiomyopathy can stem from genetic factors, infections, high blood pressure, or other underlying health conditions. The weakened or stiffened muscle struggles to meet the body’s oxygen and nutrient demands, contributing significantly to the development and progression of heart failure. Early detection and management are vital to slowing disease progression.
Arrhythmias and Heart Failure
An arrhythmia, or irregular heartbeat, profoundly impacts heart function and frequently coexists with, or even contributes to, heart failure. These irregularities occur when the electrical signals coordinating the heart’s rhythm malfunction. The heart might beat too quickly, too slowly, or erratically, diminishing its efficiency in pumping blood.
Different types of arrhythmias can arise, including atrial fibrillation, ventricular tachycardia, and bradycardia (slow heart rate). In heart failure, structural changes in the heart can disrupt these electrical pathways, fostering arrhythmia development. Conversely, sustained arrhythmias can worsen heart failure by reducing cardiac output and increasing the heart’s workload.
Managing arrhythmias is crucial in heart failure patients. Treatments range from lifestyle modifications and medications to procedures like cardioversion or implantable devices (pacemakers or defibrillators). Recognizing and addressing arrhythmias is a vital component of comprehensive heart failure care, improving symptoms and overall prognosis.
Heart Attack and its Connection to Heart Failure
A heart attack, formally known as a myocardial infarction, occurs when blood flow to a section of the heart is blocked, typically by a clot forming on pre-existing plaque buildup within the coronary arteries. This blockage deprives the heart muscle of oxygen, leading to damage or death of heart tissue.
The connection to heart failure is significant: a heart attack can directly weaken the heart muscle, reducing its ability to pump effectively. The extent of damage dictates the severity of potential heart failure. Even if the initial attack isn’t fatal, the scarred tissue left behind can impair heart function over time.

Repeated heart attacks or large-scale damage significantly increase the risk of developing chronic heart failure. Early recognition of heart attack symptoms – chest pain, shortness of breath, nausea – and prompt medical intervention are crucial to minimize damage and potentially prevent or delay the onset of heart failure;

Arteriosclerosis: A Contributing Factor
Arteriosclerosis represents a critical underlying process in the development of many heart conditions, including those leading to heart failure. It’s characterized by the thickening and stiffening of artery walls, reducing their elasticity and hindering efficient blood flow throughout the body. This diminished blood supply impacts the heart’s ability to receive the oxygen and nutrients it needs to function optimally.
Fatty deposits, known as plaques, gradually accumulate within the arteries over time, a process often linked to lifestyle factors like diet and lack of exercise. These plaques narrow the arteries, further restricting blood flow and increasing the heart’s workload. As the condition progresses, it can lead to both heart attack and heart failure.
Managing arteriosclerosis through lifestyle modifications – a low-salt diet, regular exercise – and medical interventions is vital. Addressing this condition proactively can significantly reduce the risk of developing heart failure and improve overall cardiovascular health, promoting long-term well-being.
Symptoms of LMNOP Heart Failure
Recognizing the symptoms of heart failure is paramount for early intervention and improved outcomes. A core characteristic is the heart’s inability to pump blood effectively, leading to a backup of fluid within the lungs and extremities. This manifests in several noticeable ways, often developing gradually.
Common symptoms include shortness of breath, particularly during exertion or when lying down, and persistent coughing or wheezing due to fluid accumulation in the lungs. Swelling in the ankles, feet, and legs – known as edema – is another frequent sign, indicating fluid retention. Fatigue and weakness are also prevalent, as the heart struggles to meet the body’s demands.
Furthermore, individuals may experience an irregular heartbeat (arrhythmia) or a sensation of fluttering in the chest. It’s crucial to be vigilant for these signs and seek medical attention promptly if they arise, as early diagnosis and treatment can significantly impact the progression of the condition and enhance quality of life.
Early Warning Signs
Detecting the subtle early warning signs of LMNOP heart failure is critical for proactive management and preventing disease progression. Often, these initial indicators are easily dismissed or attributed to other causes, delaying crucial medical attention. Paying close attention to bodily changes is key.
One of the first signs can be unexplained fatigue, even after adequate rest. This stems from the heart’s reduced ability to efficiently circulate blood, depriving muscles of necessary oxygen. Shortness of breath during routine activities, like climbing stairs or walking, is another red flag. Noticeable swelling in the ankles and feet, particularly at the end of the day, suggests fluid retention.
Additionally, a persistent cough, especially when lying down, or an increased need to urinate at night could signal fluid buildup in the lungs. Any new or worsening palpitations or an irregular heartbeat should also be investigated. Recognizing these early cues and consulting a healthcare professional promptly can lead to timely diagnosis and intervention, improving long-term outcomes.
Recognizing Fluid Buildup
Fluid buildup is a hallmark symptom of LMNOP heart failure, occurring when the heart’s diminished pumping capacity causes blood to back up, increasing pressure in the veins and capillaries. This forces fluid into surrounding tissues, leading to noticeable swelling – edema – in various parts of the body.
Peripheral edema, commonly observed in the ankles, feet, and legs, is often the first noticeable sign. This swelling typically worsens throughout the day and improves with elevation. Pulmonary edema, fluid accumulation in the lungs, manifests as shortness of breath, particularly when lying flat, and a persistent cough, potentially producing frothy sputum.

Abdominal swelling, known as ascites, can also occur due to fluid buildup in the peritoneal cavity. Weight gain from fluid retention is another important indicator. Regularly monitoring weight and being vigilant for these physical changes are crucial for managing LMNOP heart failure. Promptly reporting any significant fluid buildup to a healthcare provider is essential for adjusting treatment and preventing complications.

Bradycardia and its Impact
Bradycardia, defined as a slow heart rate – fewer than 60 beats per minute in adults at rest – can significantly impact individuals with LMNOP heart failure. While a slower heart rate isn’t inherently problematic for everyone, in the context of heart failure, it can exacerbate symptoms and reduce the heart’s already compromised ability to effectively circulate blood.

A reduced heart rate means less blood is pumped with each beat, potentially leading to fatigue, weakness, dizziness, and shortness of breath. In severe cases, bradycardia can cause fainting or even cardiac arrest. It’s crucial to understand that bradycardia isn’t always a cause of heart failure, but it can be a complicating factor, particularly if the underlying heart muscle is weakened.
Management of bradycardia in heart failure often involves identifying the underlying cause and potentially implanting a pacemaker to regulate the heart rhythm. Regular monitoring and communication with a healthcare provider are vital to ensure appropriate treatment and prevent adverse effects.
Diagnosis of LMNOP Heart Failure
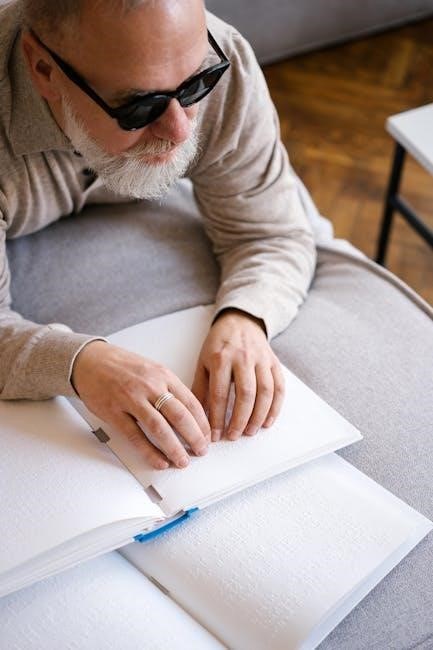
Accurate diagnosis of LMNOP heart failure is paramount for effective management and improved patient outcomes. The diagnostic process typically involves a comprehensive evaluation, beginning with a detailed medical history and physical examination to assess symptoms like shortness of breath and fluid retention.
Several diagnostic tests are employed to confirm the diagnosis and determine the severity of the condition. These include an echocardiogram, which provides images of the heart’s structure and function; an electrocardiogram (ECG) to detect arrhythmias; and blood tests to measure levels of natriuretic peptides, indicators of heart strain.
Further procedures may include a chest X-ray to check for fluid in the lungs, and potentially a cardiac MRI or catheterization to provide more detailed information about the heart’s anatomy and performance. Early and precise diagnosis allows for timely intervention and personalized treatment plans.
Diagnostic Tests and Procedures
A range of tests and procedures are utilized to accurately diagnose LMNOP heart failure and assess its severity. Echocardiograms are fundamental, providing detailed images of the heart’s structure and function, revealing any abnormalities in pumping ability or valve function. An electrocardiogram (ECG) detects irregular heartbeats, or arrhythmias, which often accompany heart failure.
Blood tests play a crucial role, specifically measuring levels of natriuretic peptides – biomarkers released when the heart is strained. Chest X-rays help identify fluid buildup in the lungs, a common symptom. More advanced imaging, like cardiac MRI, offers detailed anatomical views, while cardiac catheterization directly assesses heart pressures and function.
These procedures help differentiate between types of heart failure and guide treatment decisions. Accurate diagnosis is essential for tailoring a personalized management plan and improving patient prognosis, ensuring optimal care and well-being.
Treatment Options for LMNOP Heart Failure
Treatment for LMNOP heart failure is multifaceted, tailored to the individual’s specific condition and severity. Lifestyle changes are foundational, including a diet low in sodium and regular, moderate exercise, as recommended by a healthcare professional. Medications form a cornerstone of therapy, with options like ACE inhibitors, beta-blockers, and diuretics to manage symptoms and improve heart function.
Emerging therapies, such as polypills – combinations of essential heart failure medications – are gaining attention for their potential to simplify treatment regimens and improve adherence. Addressing underlying conditions like arrhythmias or arteriosclerosis is also vital. In severe cases, devices like pacemakers or implantable cardioverter-defibrillators (ICDs) may be considered to regulate heart rhythm.
Ultimately, the goal is to alleviate symptoms, slow disease progression, and enhance quality of life. A collaborative approach between patients and healthcare providers is crucial for optimal outcomes.

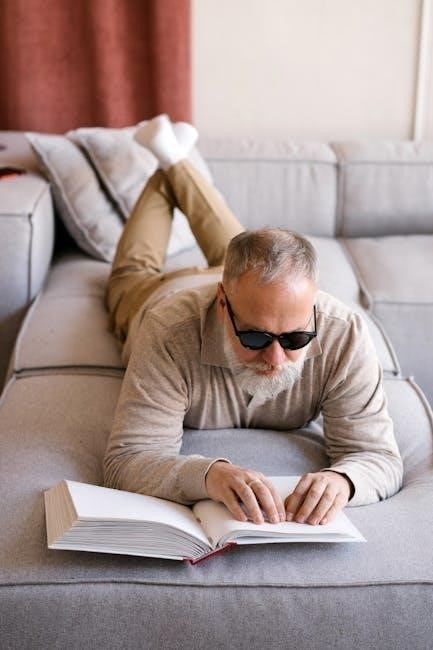
Lifestyle Changes: Diet and Exercise
Adopting heart-healthy lifestyle habits is paramount in managing LMNOP heart failure. Dietary modifications are crucial, emphasizing a low-sodium intake to minimize fluid retention and reduce the heart’s workload. Focus on fruits, vegetables, whole grains, and lean proteins. Limiting processed foods, saturated fats, and cholesterol is also essential.
Regular exercise, tailored to individual capabilities, plays a vital role. Moderate-intensity activities like walking, cycling, or swimming can improve cardiovascular fitness and strengthen the heart muscle. However, it’s crucial to consult a healthcare professional before starting any new exercise program.
Maintaining a healthy weight and avoiding smoking are equally important. Stress management techniques, such as yoga or meditation, can also contribute to overall well-being. These changes, while seemingly small, collectively offer significant benefits in managing LMNOP heart failure and improving quality of life.
New Drugs and Therapies (Polypills)
The landscape of heart failure treatment is evolving, with promising new drugs and therapies emerging. While still under investigation, polypills – combining multiple medications into a single dose – are gaining attention as a potential game-changer. Experts are actively preparing for their introduction, even before conclusive randomized trial data is available.

These polypills aim to simplify medication regimens and improve adherence, a significant challenge for many heart failure patients. Current treatment strategies often involve a combination of drugs targeting different aspects of the condition, such as blood pressure control, fluid management, and heart muscle function.
Ongoing research focuses on developing novel therapies that address the underlying causes of heart failure and promote heart muscle recovery. A growing awareness of the condition, coupled with these advancements, offers renewed hope for improved outcomes and a better quality of life for those living with LMNOP heart failure.
Preventative Measures and Long-Term Well-being
Proactive steps are vital in mitigating the risk and progression of LMNOP heart failure. While some risk factors, like family history, are unchangeable, significant lifestyle modifications can dramatically improve heart health. A cornerstone of prevention is adopting a diet low in salt, crucial for managing blood pressure and fluid retention.
Regular exercise, tailored to individual capabilities, strengthens the heart muscle and improves overall cardiovascular function. Early detection of symptoms, such as unexplained fatigue or swelling in the legs, is paramount. Consistent monitoring of heart rate and blood pressure, alongside regular check-ups, allows for timely intervention.
Long-term well-being necessitates adherence to prescribed medications and a commitment to a heart-healthy lifestyle. Managing stress, maintaining a healthy weight, and avoiding smoking are also essential components of a comprehensive preventative strategy. Prioritizing these measures empowers individuals to take control of their heart health and enjoy a fuller, more active life.

